Alright, buckle up buttercups, because we’re diving headfirst into the hilarious world of the ulcer diet food list pdf! Yep, that’s right, we’re talking about those pesky little stomach troublemakers and how to tame them with the power of… food! Forget boring diets; we’re here to find out how to eat your way to a happy tummy. This isn’t just about avoiding pain; it’s about becoming a culinary ninja, expertly navigating the minefield of meals to keep your insides smiling.
Get ready to learn the ins and outs of what to eat, what to avoid, and how to become a master of the meal plan!
This guide, or rather, your new best friend, the ulcer diet food list pdf, is your roadmap to a happier gut. We’ll be exploring everything from the basic principles of ulcer diets (think: gentle giants for your stomach) to the nitty-gritty details of meal timing, portion control, and even the sneaky impact of your favorite beverages. We’ll also uncover the secrets of cooking methods, supplements, and lifestyle tweaks that can make a world of difference.
And of course, we’ve got a treasure trove of recipes to get you started on your culinary adventure!
Introduction to Ulcer Diets
Ulcer diets are designed to help manage the symptoms of peptic ulcers and promote healing. They focus on modifying the diet to reduce irritation in the stomach and intestines, allowing the ulcer to heal while minimizing pain and discomfort. Understanding the principles behind this dietary approach is crucial for anyone dealing with peptic ulcers.
Understanding Peptic Ulcers
Peptic ulcers are sores that develop in the lining of the stomach, small intestine, or esophagus. These ulcers occur when the protective lining of the digestive tract is eroded, exposing the underlying tissue to stomach acid.The primary causes of peptic ulcers include:
- Infection with Helicobacter pylori (H. pylori) bacteria: This is the most common cause. The bacteria damages the protective lining.
- Long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs): These medications, such as ibuprofen and aspirin, can irritate the stomach lining.
- Excessive stomach acid production: Although less common, conditions that increase acid production can contribute to ulcer formation.
Dietary Role in Ulcer Management
Diet plays a significant role in managing ulcer symptoms and promoting healing. The goal of an ulcer diet is to reduce stomach acid production, soothe the irritated lining of the digestive tract, and prevent further damage. This is achieved by selecting foods that are easy to digest and avoiding those that can worsen symptoms.The diet focuses on:
- Avoiding Irritants: This includes foods and beverages that stimulate acid production or directly irritate the ulcer.
- Choosing Soothing Foods: These are generally bland, easy-to-digest foods that are gentle on the stomach.
- Eating Regular Meals: Eating small, frequent meals can help to buffer stomach acid and prevent the stomach from becoming overly full.
Foods to Include in an Ulcer Diet
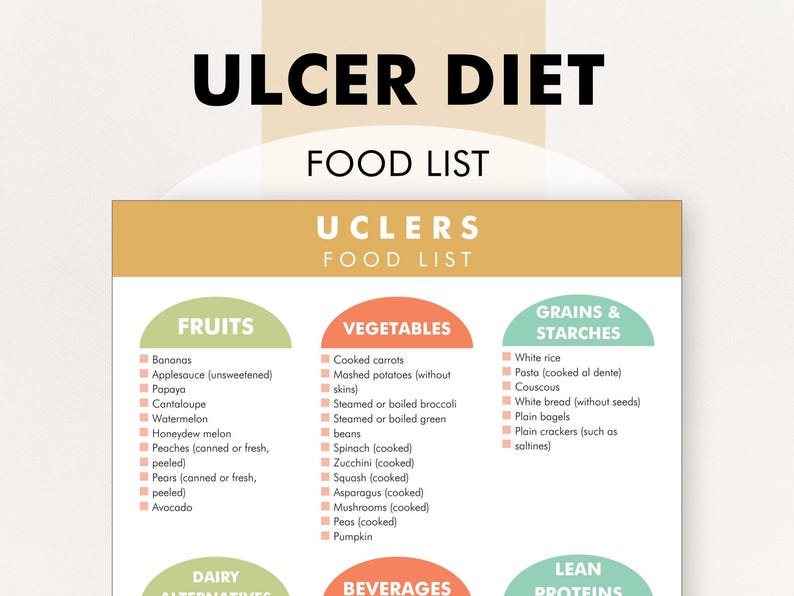
Following an ulcer diet focuses on foods that soothe the stomach lining and minimize acid production. This section details food choices generally considered safe and beneficial for those managing ulcers. The goal is to provide a diet that supports healing and reduces discomfort.
Choosing the right foods is crucial for managing ulcers. The following foods are generally well-tolerated and can aid in the healing process. They are selected for their low acidity, ease of digestion, and potential to protect the stomach lining. Remember to consult your doctor or a registered dietitian for personalized advice.
Foods Considered Safe and Beneficial
This list presents foods that are generally well-tolerated by individuals with ulcers. These choices prioritize ease of digestion and minimal irritation to the stomach lining. Consider these options as part of a balanced meal plan.
Browse the multiple elements of starchless as some foods to gain a more broad understanding.
- Lean Proteins: Chicken (skinless), turkey, fish (baked or grilled, not fried), tofu, and egg whites. These proteins are easier to digest than red meat and provide essential amino acids.
- Dairy (in moderation): Low-fat yogurt, milk, and cheese. Some individuals find dairy products soothing, while others may experience increased discomfort. Pay attention to your body’s response.
- Healthy Fats: Olive oil, avocados, and small amounts of nuts and seeds. These fats are less likely to trigger acid reflux than saturated or trans fats.
- Whole Grains: Oatmeal, brown rice, whole-wheat bread (in moderation). Choose whole grains for their fiber content, but be mindful of portion sizes.
- Non-Citrus Fruits: Bananas, applesauce, melons (cantaloupe, honeydew), and pears. These fruits are generally low in acidity and easy to digest.
- Cooked Vegetables: Carrots, green beans, spinach, and sweet potatoes. Cooking vegetables softens their fibers, making them easier on the stomach.
- Beverages: Water, herbal teas (non-caffeinated). Staying hydrated is essential. Avoid caffeine and alcohol.
Fruits and Vegetables for an Ulcer Diet
Selecting the right fruits and vegetables is essential for an ulcer diet. The table below provides examples of suitable options, emphasizing low-acid content and ease of digestion. These choices support healing and minimize irritation.
| Fruits | Vegetables |
|---|---|
|
|
Rationale Behind Food Choices
The foods recommended in an ulcer diet are selected based on their properties. They are generally low in acidity, easy to digest, and gentle on the stomach lining. Understanding the rationale helps in making informed dietary choices.
Low-acid foods reduce stomach irritation, while easily digestible options minimize the workload on the digestive system.
These foods are chosen to reduce the symptoms associated with ulcers. For instance, fruits like bananas are naturally low in acid and can help to soothe the stomach. Cooked vegetables are easier to digest than raw ones, reducing the strain on the digestive system. Lean proteins provide essential nutrients without being overly difficult to process.
Meal Planning Ideas
Incorporating these foods into meal planning is essential for a successful ulcer diet. Here are some meal ideas that integrate the recommended foods.
Breakfast: Oatmeal with a banana and a small amount of low-fat yogurt. This combination provides fiber, potassium, and probiotics, all beneficial for digestive health. Another option is a whole-wheat toast with egg whites and avocado slices.
Lunch: Grilled chicken salad with spinach, carrots, and a light olive oil dressing. This provides lean protein and easily digestible vegetables. Another option is a turkey sandwich on whole-wheat bread with lettuce and avocado.
Dinner: Baked fish with steamed green beans and sweet potatoes. This meal is rich in protein, vitamins, and minerals while being easy on the stomach. Another option is tofu stir-fry with brown rice and cooked vegetables.
Snacks: Applesauce, a small handful of almonds, or a small serving of low-fat yogurt. These snacks provide nutrients and help to prevent hunger without irritating the stomach. It is important to eat small meals and snacks throughout the day to avoid long periods without food.
Foods to Avoid with Ulcers
Managing an ulcer involves more than just including beneficial foods; it also requires carefully avoiding those that can exacerbate symptoms and hinder healing. This section Artikels foods that are commonly known to irritate ulcers, along with insights into why they pose a problem and how to identify them on food labels.
Understanding and avoiding these trigger foods is crucial for effective ulcer management and promoting a more comfortable experience.
Foods That Commonly Irritate Ulcers
Certain foods and beverages can significantly worsen ulcer symptoms. Here’s a list of commonly problematic items:
- Spicy Foods: Chili peppers, hot sauces, and foods with high levels of capsaicin can irritate the stomach lining.
- Acidic Foods: Citrus fruits (oranges, lemons, grapefruits), tomatoes, and vinegar-based products can increase stomach acidity.
- Caffeinated Beverages: Coffee, tea, and energy drinks can stimulate acid production.
- Alcoholic Beverages: Alcohol can erode the stomach lining and increase acid production.
- Fried and Fatty Foods: These can slow digestion and potentially irritate the stomach.
- Processed Foods: Often high in salt, sugar, and additives that may irritate the stomach.
- Carbonated Beverages: Sodas and other fizzy drinks can cause bloating and discomfort.
- Chocolate: Contains caffeine and other compounds that can stimulate acid production.
- Certain Dairy Products: Some individuals find that high-fat dairy products worsen symptoms.
Comparing Safe and Unsafe Foods for Ulcers
This table provides a side-by-side comparison to help you easily identify which foods are generally considered safe and which should be avoided when managing an ulcer. The table is designed for easy viewing on various devices.
| Safe Foods | Unsafe Foods | Reason for Safety | Reason for Avoidance |
|---|---|---|---|
| Non-citrus fruits (bananas, apples) | Citrus fruits (oranges, lemons) | Low acidity, gentle on the stomach | High acidity can irritate the ulcer |
| Lean proteins (chicken, fish) | Fatty meats, fried foods | Easy to digest, minimal stomach irritation | Can slow digestion and irritate the stomach |
| Cooked vegetables (carrots, green beans) | Raw vegetables (especially those high in fiber) | Easier to digest, less likely to cause discomfort | Can cause bloating and potentially increase stomach acid |
| Non-caffeinated beverages (water, herbal tea) | Caffeinated beverages (coffee, tea) | Do not stimulate acid production | Can stimulate acid production, potentially worsening symptoms |
Reasons for Avoiding Certain Foods
Understanding the underlying reasons why specific foods should be avoided can empower you to make informed dietary choices and better manage your ulcer. Key factors include acidity levels, spice content, and their impact on digestion.
- High Acidity: Foods like citrus fruits, tomatoes, and vinegar can increase stomach acidity, irritating the ulcer and causing pain.
- Spice Levels: Spicy foods contain compounds like capsaicin, which can directly irritate the stomach lining, leading to inflammation and discomfort.
- Fat Content: High-fat foods can slow down digestion, which can increase the time food spends in the stomach, potentially exacerbating symptoms.
- Caffeine and Alcohol: Both caffeine and alcohol stimulate acid production, which can worsen ulcer symptoms and hinder healing.
- Irritants and Additives: Processed foods often contain additives and high levels of salt and sugar that can irritate the stomach lining and disrupt the digestive process.
Reading Food Labels to Identify Problematic Ingredients
Food labels are essential tools for making informed choices about what you eat. Learning to read them carefully can help you identify ingredients that might trigger your ulcer symptoms. This is especially important for packaged and processed foods.
- Check for Acidic Ingredients: Look for ingredients like citric acid, vinegar, and tomato paste, which indicate higher acidity levels.
- Identify Spices and Flavorings: Be aware of ingredients such as chili powder, cayenne pepper, and hot sauce, which can irritate the stomach.
- Assess Fat Content: Pay attention to the total fat and saturated fat content, as high levels can slow digestion.
- Review Caffeine Content: Check for ingredients like coffee, tea, or guarana, which indicate caffeine.
- Be Mindful of Additives: Look for artificial flavors, colors, and preservatives, as some individuals find these irritating.
- Examine Sugar and Salt Levels: Excessive sugar and salt can also cause digestive issues.
- Consider Serving Sizes: Be aware of the serving size and how it relates to the nutritional information provided.
By diligently reading food labels and being mindful of ingredients, you can make choices that support your ulcer management plan.
Meal Timing and Portion Control
Maintaining a consistent eating schedule and managing portion sizes are crucial components of an ulcer diet. These practices help regulate stomach acid production and minimize irritation to the ulcerated lining. Careful attention to meal timing and portion control can significantly alleviate symptoms and promote healing.
Importance of Meal Frequency and Timing, Ulcer diet food list pdf
Regular meal times are essential for managing ulcers. Irregular eating patterns can lead to fluctuations in stomach acid levels, potentially exacerbating symptoms. Consistent timing helps maintain a more stable environment within the stomach, reducing the likelihood of acid irritating the ulcer.
Ideal Meal Schedule for Ulcer Patients
The ideal meal schedule for ulcer patients typically involves frequent, smaller meals throughout the day. This approach prevents the stomach from becoming overly full and reduces the production of excess stomach acid. It also ensures a constant supply of nutrients for healing.
- Breakfast: Consume a light breakfast within an hour of waking up.
- Mid-Morning Snack: Have a small snack about 2-3 hours after breakfast.
- Lunch: Eat lunch approximately 2-3 hours after the mid-morning snack.
- Afternoon Snack: Another small snack 2-3 hours after lunch.
- Dinner: Have a light dinner 2-3 hours before bedtime.
- Bedtime Snack (Optional): A small, easily digestible snack before bed can help neutralize stomach acid produced overnight.
Tips on Appropriate Portion Sizes
Appropriate portion sizes are critical to prevent overeating and discomfort. Overeating can increase stomach acid production and put pressure on the stomach, potentially worsening ulcer symptoms. Smaller, more frequent meals are the key.
- Use smaller plates: This can help you visually control portion sizes.
- Eat slowly: Allow time for your body to register fullness.
- Listen to your body: Stop eating when you feel satisfied, not overly full.
- Avoid second helpings: Resist the temptation to eat more than your initial portion.
- Measure your food: Use measuring cups and spoons to ensure accurate portion sizes, especially in the beginning.
Sample Meal Plan for a Day
Here’s a sample meal plan illustrating the meal timing and portion sizes recommended for ulcer patients. This is a general guideline, and individual needs may vary. Always consult with a healthcare professional or a registered dietitian to personalize your meal plan.
| Meal | Time | Portion Size | Example Foods |
|---|---|---|---|
| Breakfast | 7:00 AM | 1 cup | Oatmeal (1/2 cup) with banana slices (1/2 cup) and a small glass of milk (1/2 cup) |
| Mid-Morning Snack | 9:30 AM | 1/2 cup | Plain yogurt (1/2 cup) |
| Lunch | 12:00 PM | 1.5 cups | Grilled chicken breast (3 oz), cooked white rice (1/2 cup), steamed carrots (1/2 cup) and a small side salad (1/2 cup) with a light vinaigrette |
| Afternoon Snack | 2:30 PM | 1/2 cup | A few whole-wheat crackers (4-5) with a slice of low-fat cheese. |
| Dinner | 6:00 PM | 1.5 cups | Baked cod (3 oz), baked potato (1/2 cup) with a small amount of butter and steamed green beans (1/2 cup) |
| Bedtime Snack (Optional) | 8:30 PM | 1/2 cup | A small bowl of cooked applesauce (1/2 cup). |
Beverages and Ulcer Diets
Beverages play a significant role in managing ulcer symptoms. Choosing the right drinks can soothe the stomach and aid healing, while others can exacerbate discomfort and delay recovery. Understanding the impact of different beverages is crucial for anyone following an ulcer diet. This section will guide you through the best and worst choices, including the effects of alcohol and caffeine.
Impact of Beverages on Ulcer Symptoms
Certain beverages can irritate the stomach lining, increasing acid production and worsening ulcer symptoms like pain, heartburn, and nausea. Conversely, other drinks can be soothing and may even promote healing. It is important to pay attention to how different beverages affect your body and adjust your intake accordingly.
Safe and Avoidable Beverages
Here’s a breakdown of beverages generally considered safe and those that should be avoided when managing an ulcer:
- Generally Safe Beverages:
- Water: The cornerstone of any healthy diet, water helps with hydration and can dilute stomach acid.
- Herbal Teas (non-caffeinated): Chamomile, ginger, and licorice root teas are often recommended for their soothing properties. Avoid teas with added citric acid.
- Milk (in moderation): Milk can temporarily buffer stomach acid, but some people find it can later stimulate acid production. Opt for low-fat or non-fat varieties.
- Coconut Water: This natural beverage is a good source of electrolytes and can be gentle on the stomach.
- Rice Milk and Oat Milk: These are generally well-tolerated alternatives to dairy milk.
- Beverages to Avoid:
- Coffee: Coffee is a significant acid producer and can worsen ulcer symptoms.
- Alcohol: Alcohol can irritate the stomach lining and increase acid production.
- Carbonated Drinks: The bubbles in carbonated drinks can cause bloating and discomfort.
- Citrus Juices: Orange, grapefruit, and other citrus juices are highly acidic and can irritate ulcers.
- Tomato Juice: Tomatoes are acidic and should be avoided.
- Energy Drinks: Often high in caffeine and other stimulants, energy drinks can exacerbate symptoms.
Effects of Alcohol and Caffeine on Ulcers
Alcohol and caffeine are two of the most problematic substances for people with ulcers.
- Alcohol: Alcohol directly irritates the stomach lining, causing inflammation and increasing acid production. It can also interfere with the healing process and may increase the risk of bleeding. Even moderate alcohol consumption can be detrimental.
- Caffeine: Caffeine, found in coffee, tea, and some soft drinks, stimulates the production of stomach acid. This excess acid can erode the protective lining of the stomach and duodenum, worsening ulcer symptoms. The effect of caffeine can vary from person to person, but it’s generally best to limit or eliminate it.
Beverage Suitability for an Ulcer Diet
The table below summarizes the suitability of various beverages for an ulcer diet, helping you make informed choices.
| Beverage | Suitability | Notes |
|---|---|---|
| Water | Suitable | Essential for hydration and dilution of stomach acid. |
| Herbal Tea (Chamomile, Ginger, Licorice Root) | Suitable | Soothing and may reduce inflammation; choose caffeine-free options. |
| Milk (Low-Fat/Non-Fat) | Generally Suitable (in moderation) | Can temporarily buffer stomach acid, but monitor for increased acid production later. |
| Coconut Water | Suitable | Good source of electrolytes and easy on the stomach. |
| Rice Milk and Oat Milk | Suitable | Well-tolerated alternatives to dairy milk. |
| Coffee | Avoid | Highly acidic; stimulates acid production. |
| Alcohol | Avoid | Irritates stomach lining and increases acid production. |
| Carbonated Drinks | Avoid | Can cause bloating and discomfort. |
| Citrus Juices | Avoid | Highly acidic and irritating. |
| Tomato Juice | Avoid | Acidic and can exacerbate symptoms. |
| Energy Drinks | Avoid | High in caffeine and stimulants; can worsen symptoms. |
Cooking Methods and Preparation
Preparing food correctly is crucial for managing ulcers. The way you cook food can significantly impact its tolerability and how it affects your stomach. Choosing gentle cooking methods can make your meals more comfortable and help with healing.
Impact of Cooking Methods on Food Tolerability
Different cooking techniques affect food’s texture, digestibility, and the potential for irritation. High-heat methods can create compounds that might exacerbate ulcer symptoms, while gentler methods preserve nutrients and make food easier to digest.
Gentle Cooking Methods for Ulcer Patients
Prioritizing certain cooking methods can make a big difference in managing ulcer symptoms.
- Steaming: Steaming uses gentle heat and preserves nutrients. Vegetables like broccoli and carrots become tender without losing their beneficial properties.
- Boiling: Boiling is a simple method, especially suitable for preparing plain foods like rice or pasta. Ensure food is cooked until soft.
- Braising: Braising combines browning with slow simmering in liquid. This tenderizes meats and infuses flavors gently.
- Poaching: Poaching involves cooking food in a liquid at a low temperature. It’s ideal for delicate foods like eggs or fish, making them easy to digest.
- Microwaving: Microwaving is quick and preserves nutrients. Use it to cook vegetables or reheat meals.
Recipe Modifications for Ulcer-Friendly Meals
Modifying existing recipes can make them suitable for an ulcer diet. This often involves adjusting ingredients and cooking techniques.
- Reduce Fat: High-fat foods can irritate the stomach. Use lean proteins, and trim visible fat from meats.
- Avoid Acidic Ingredients: Tomatoes, citrus fruits, and vinegar can worsen symptoms. Substitute them with milder alternatives.
- Cook Until Tender: Ensure that foods are thoroughly cooked to make them easier to digest.
- Season Mildly: Avoid spicy seasonings, and use herbs and mild spices in moderation.
- Use Gentle Cooking Methods: Prioritize steaming, boiling, or poaching over frying or grilling.
For example, if a recipe calls for a tomato-based sauce, you could replace it with a cream-based sauce or a sauce made from cooked, pureed vegetables like carrots or zucchini. If a recipe calls for grilling a steak, you can try braising or poaching a lean cut of meat instead.
Cooking Tips for Preparing Meals
- Choose Fresh Ingredients: Fresh, whole foods are generally better tolerated than processed foods.
- Prepare Meals in Advance: Planning and preparing meals ahead of time can help you stick to your diet and avoid making impulsive, less healthy choices.
- Cook in Batches: Cooking large batches of food allows you to freeze portions for later use, ensuring you always have ulcer-friendly meals available.
- Experiment with Flavors: Use herbs and mild spices to add flavor without irritating your stomach. Examples include basil, oregano, and turmeric.
- Pay Attention to Portion Sizes: Eating smaller, more frequent meals can reduce the burden on your stomach.
Supplements and Ulcer Management: Ulcer Diet Food List Pdf
Supplements can play a supporting role in managing and potentially healing ulcers. They are not a replacement for medical treatment or dietary changes, but can provide additional support to the body. Always consult with a healthcare professional before starting any new supplement regimen, especially if you are taking other medications. The effectiveness of supplements can vary, and individual responses can differ.
Beneficial Supplements for Ulcer Healing
Certain supplements may aid in ulcer healing and symptom relief. They work through various mechanisms, such as reducing inflammation, promoting tissue repair, and combating bacteria. However, it’s essential to understand that research on the effectiveness of these supplements is ongoing, and more studies are needed to confirm their benefits and optimal dosages.
- Probiotics: These beneficial bacteria can help restore the balance of gut flora, which may be disrupted in people with ulcers. Probiotics can reduce
-H. pylori* infection, a major cause of peptic ulcers, and improve digestive health. Studies have shown that certain probiotic strains can help eradicate
-H. pylori* when used in conjunction with standard antibiotic therapy.For instance, a meta-analysis of several studies indicated that probiotics containing strains like
-Lactobacillus* and
-Bifidobacterium* significantly improved
-H. pylori* eradication rates and reduced side effects associated with antibiotics. - L-Glutamine: This amino acid is a crucial fuel source for cells in the gut lining and can aid in tissue repair and reduce inflammation. Glutamine supplementation may help strengthen the gut barrier and accelerate the healing of ulcers. Research suggests that glutamine can increase the production of heat shock proteins, which help protect cells from damage. In clinical settings, L-glutamine is sometimes used to manage conditions like leaky gut syndrome, which can be associated with ulcer development.
- Zinc: Zinc is essential for wound healing and immune function. Zinc deficiency can impair the body’s ability to repair damaged tissues. Some studies suggest that zinc supplementation can accelerate the healing of ulcers. Zinc has been shown to stimulate the production of growth factors, which are essential for tissue repair. In a study published in the “Journal of Gastroenterology and Hepatology,” zinc supplementation was found to improve ulcer healing rates in patients with peptic ulcers.
- Licorice Root (Deglycyrrhizinated Licorice – DGL): DGL licorice is a form of licorice root that has the glycyrrhizin removed, which prevents side effects such as high blood pressure. DGL can stimulate the production of protective mucus in the stomach lining, helping to protect against acid damage and promote ulcer healing. DGL is believed to increase the levels of prostaglandins, which play a role in protecting the stomach lining.
In a randomized, double-blind, placebo-controlled trial, DGL was shown to be as effective as certain medications in healing peptic ulcers.
- Aloe Vera: Aloe vera has anti-inflammatory and wound-healing properties. It may help reduce inflammation and promote the healing of ulcers. Aloe vera contains compounds like polysaccharides that have been shown to stimulate the production of fibroblasts, cells that play a crucial role in wound healing. Aloe vera juice has been traditionally used to soothe digestive issues and may provide relief from ulcer symptoms.
- Vitamin C: Vitamin C is an antioxidant that can protect the stomach lining from damage and support immune function. It is essential for collagen synthesis, which is crucial for tissue repair. Vitamin C may help eradicate
-H. pylori* and improve ulcer healing rates. Studies have indicated that vitamin C supplementation can reduce the risk of developing peptic ulcers.
Potential Risks of Supplement Use
While supplements can offer potential benefits, it’s crucial to be aware of potential risks and side effects. Supplements can interact with medications, and some may cause adverse reactions. Always consult with a healthcare provider before starting any new supplement.
- Interactions with Medications: Some supplements can interact with medications, reducing their effectiveness or increasing the risk of side effects. For example, St. John’s Wort can interfere with the effectiveness of certain antidepressants, while Vitamin K can reduce the effects of blood thinners like warfarin.
- Side Effects: Supplements can cause various side effects, ranging from mild digestive upset to more serious reactions. Probiotics may cause gas or bloating, while excessive zinc intake can lead to nausea and vomiting.
- Dosage Concerns: Taking too much of a supplement can be harmful. It’s essential to follow recommended dosages and avoid exceeding the upper limits. For example, excessive intake of Vitamin C can lead to diarrhea, while too much Vitamin A can cause liver damage.
- Quality Control: The supplement industry is not as strictly regulated as the pharmaceutical industry. It’s important to choose supplements from reputable brands that undergo third-party testing to ensure product purity and potency.
- Contraindications: Some supplements may not be suitable for everyone. For instance, people with certain medical conditions, such as kidney disease or liver problems, may need to avoid certain supplements. Pregnant or breastfeeding women should also exercise caution and consult with their healthcare provider before taking any supplements.
Supplement Dosage Recommendations and Considerations
Dosage recommendations can vary depending on the supplement and individual needs. It’s essential to follow the manufacturer’s instructions and consult with a healthcare professional for personalized guidance.
- Probiotics: Dosage can vary depending on the strain and product. Typically, dosages range from 1 billion to 10 billion colony-forming units (CFUs) per day. It is often recommended to start with a lower dose and gradually increase it as tolerated.
- L-Glutamine: The typical dosage for ulcer management is between 5 to 10 grams per day, often divided into multiple doses.
- Zinc: The recommended daily dosage is typically 15-30 mg. It’s best to take zinc with food to minimize the risk of nausea.
- DGL Licorice: The typical dosage is 250-500 mg, taken 20 minutes before meals.
- Aloe Vera: Aloe vera juice can be taken in doses of 1-2 ounces, once or twice daily.
- Vitamin C: The recommended daily dosage is 500-1000 mg. It can be taken in divided doses throughout the day.
It’s important to note that these are general recommendations, and individual needs may vary. Always consult with a healthcare professional before starting any new supplement regimen.
Lifestyle Factors and Ulcer Control
Managing ulcers effectively extends beyond dietary adjustments. Lifestyle choices significantly impact ulcer symptoms and healing. Addressing stress, smoking, and alcohol consumption is crucial for overall well-being and ulcer management.
Impact of Stress on Ulcer Symptoms
Stress can exacerbate ulcer symptoms. It increases stomach acid production, potentially delaying healing and worsening pain. This effect is mediated by the nervous system, which influences digestive processes.
Managing Stress and Promoting Relaxation
Effective stress management techniques are essential for ulcer control. Incorporating these practices into daily life can significantly reduce symptoms and promote healing.
- Mindfulness Meditation: Practicing mindfulness, such as focusing on the present moment, has been shown to reduce stress levels. Regular meditation can help calm the nervous system and decrease stomach acid production. For example, studies have indicated that even 10-15 minutes of daily meditation can lead to noticeable reductions in stress hormone levels, like cortisol.
- Deep Breathing Exercises: Deep, diaphragmatic breathing can activate the parasympathetic nervous system, promoting relaxation. This can help counteract the effects of stress on the digestive system. An example of this technique involves inhaling slowly through the nose for a count of four, holding the breath for a count of four, and exhaling slowly through the mouth for a count of six.
- Regular Exercise: Physical activity releases endorphins, which have mood-boosting effects. Exercise also helps manage stress and improve overall health. Even moderate exercise, like a brisk 30-minute walk three times a week, can contribute to stress reduction.
- Adequate Sleep: Prioritizing sleep is crucial for stress management and healing. Aim for 7-9 hours of quality sleep each night. Lack of sleep can worsen stress levels and negatively impact the body’s ability to heal.
- Yoga and Tai Chi: These practices combine physical postures, breathing techniques, and meditation, offering a holistic approach to stress reduction. They can improve both physical and mental well-being, thereby reducing the impact of stress on ulcers.
Avoiding Smoking and Excessive Alcohol Consumption
Smoking and excessive alcohol consumption are detrimental to ulcer healing and overall health. They directly irritate the stomach lining and hinder the healing process.
- Smoking’s Impact: Smoking increases stomach acid production, impairs blood flow to the stomach, and slows ulcer healing. It also increases the risk of ulcer recurrence. Quitting smoking is one of the most important steps for ulcer management. According to the National Institutes of Health (NIH), smokers are twice as likely to develop peptic ulcers compared to non-smokers.
- Alcohol’s Impact: Excessive alcohol consumption can erode the stomach lining, leading to inflammation and increasing the risk of ulcers. Alcohol can also interfere with the healing process. Moderate alcohol consumption, if any, is recommended. The American College of Gastroenterology recommends limiting alcohol intake to one drink per day for women and two drinks per day for men.
Lifestyle Modifications
Making specific lifestyle changes can support ulcer management and improve overall health. These modifications can reduce symptoms and promote healing.
- Regular Eating Schedule: Maintaining a consistent eating schedule, avoiding skipping meals, can help regulate stomach acid production.
- Hydration: Drinking plenty of water throughout the day helps maintain overall health and aids digestion.
- Limit Caffeine: Excessive caffeine intake can increase stomach acid production.
- Avoid Irritants: Identify and avoid foods or substances that trigger symptoms.
- Stress Management Techniques: Incorporate stress-reducing practices into your daily routine.
- Regular Check-ups: Follow up with your healthcare provider for regular check-ups and monitoring of your condition.
Recipes for an Ulcer Diet
Following an ulcer diet doesn’t mean sacrificing flavor or variety. With careful ingredient selection and preparation, you can enjoy delicious and soothing meals that support healing and minimize discomfort. This section provides a collection of recipes designed specifically for an ulcer diet, covering breakfast, lunch, dinner, and snacks. Each recipe includes nutritional information to help you monitor your intake and ensure you’re meeting your dietary needs.Here are some delicious and ulcer-friendly recipes, categorized for different meal times:
Breakfast Recipes
Breakfast is a crucial meal, providing energy and setting the tone for the day. These recipes are gentle on the stomach and packed with nutrients.* Creamy Oatmeal with Banana and Honey: Prepare oatmeal with water or low-fat milk. Add sliced banana and a drizzle of honey. Nutritional Information (per serving): Calories: 250, Protein: 8g, Carbohydrates: 45g, Fat: 4g.* Scrambled Eggs with Whole Wheat Toast: Scramble two eggs with a touch of olive oil.
Serve with a slice of whole-wheat toast. Nutritional Information (per serving): Calories: 280, Protein: 15g, Carbohydrates: 25g, Fat: 12g.* Smoothie with Banana, Yogurt, and Spinach: Blend one banana, ½ cup of plain yogurt, a handful of spinach, and a splash of water. Nutritional Information (per serving): Calories: 200, Protein: 10g, Carbohydrates: 35g, Fat: 2g.
“Breakfast provides the necessary energy and nutrients to kickstart your metabolism and set the tone for a comfortable day. These recipes are designed to be gentle on the stomach while providing essential nutrients.”
Lunch Recipes
Lunch should be light and easy to digest. These recipes are designed to be both satisfying and ulcer-friendly.* Chicken and Rice Soup: Prepare a soup with cooked chicken breast, white rice, carrots, and celery. Season lightly with salt and pepper. Nutritional Information (per serving): Calories: 300, Protein: 25g, Carbohydrates: 30g, Fat: 8g.* Turkey and Avocado Sandwich on Whole Wheat Bread: Use thinly sliced turkey breast, mashed avocado, and whole-wheat bread.
Avoid adding acidic condiments. Nutritional Information (per serving): Calories: 350, Protein: 20g, Carbohydrates: 35g, Fat: 15g.* Baked Salmon with Steamed Asparagus: Bake salmon fillet with a drizzle of olive oil. Serve with steamed asparagus. Nutritional Information (per serving): Calories: 380, Protein: 30g, Carbohydrates: 10g, Fat: 20g.
“Lunch should be a balance of nutrients that is easy to digest. Avoiding trigger foods during lunch is especially important to prevent any discomfort.”
Dinner Recipes
Dinner can be a more substantial meal, but it should still be easy to digest. These recipes are designed to be both filling and gentle on the stomach.* Baked Chicken Breast with Mashed Potatoes: Bake chicken breast with herbs. Serve with mashed potatoes made with milk and butter. Nutritional Information (per serving): Calories: 450, Protein: 35g, Carbohydrates: 40g, Fat: 18g.* Lean Ground Beef with Rice and Green Beans: Cook lean ground beef and mix it with white rice and steamed green beans.
Nutritional Information (per serving): Calories: 400, Protein: 30g, Carbohydrates: 45g, Fat: 12g.* Pasta with Chicken and Cream Sauce: Use plain pasta, cooked chicken, and a creamy sauce made with milk and flour. Avoid tomatoes. Nutritional Information (per serving): Calories: 500, Protein: 25g, Carbohydrates: 60g, Fat: 20g.
“Dinner offers a chance to incorporate a wider variety of ingredients while still focusing on digestibility. Be mindful of portion sizes to avoid overeating before bed.”
Snack Recipes
Snacks are important for maintaining blood sugar levels and preventing hunger. These recipes are designed to be gentle on the stomach.* Plain Yogurt with a few Berries: Plain yogurt with a small amount of berries, such as blueberries or raspberries. Nutritional Information (per serving): Calories: 150, Protein: 10g, Carbohydrates: 20g, Fat: 5g.* Crackers with Cottage Cheese: Saltine crackers or plain crackers served with cottage cheese.
Nutritional Information (per serving): Calories: 200, Protein: 12g, Carbohydrates: 20g, Fat: 8g.* Banana slices: A simple banana provides a quick energy boost and is easy to digest. Nutritional Information (per serving): Calories: 100, Protein: 1g, Carbohydrates: 27g, Fat: 0g.
“Snacks can help maintain stable blood sugar levels and prevent overeating during meals. These options are light, easy to digest, and provide a good source of nutrients.”
Special Considerations
Navigating an ulcer diet requires a personalized approach. This section highlights crucial dietary adaptations for specific health conditions and life stages, ensuring optimal ulcer management alongside other health concerns. Understanding these special considerations is key to tailoring your diet for the best possible outcomes.
Ulcer Management During Pregnancy
Pregnancy necessitates careful attention to both maternal and fetal health. Dietary choices play a critical role in managing ulcers while ensuring a healthy pregnancy.
- Medication Considerations: Certain ulcer medications may be unsafe during pregnancy. Always consult with your doctor about safe alternatives. For instance, some antacids containing aluminum or magnesium are generally considered safe, while others require careful evaluation.
- Morning Sickness Management: Morning sickness can exacerbate ulcer symptoms. Eating small, frequent meals, as recommended for ulcer management, can also help alleviate nausea. Bland foods like crackers and toast can be beneficial.
- Nutrient Needs: Ensure adequate intake of essential nutrients, crucial for both mother and baby. Iron, folic acid, and calcium are particularly important. Your doctor may recommend supplements, especially if dietary restrictions limit your intake of these nutrients.
- Food Safety: Be extra cautious about food safety to avoid foodborne illnesses, which can worsen ulcer symptoms and pose risks during pregnancy. Avoid undercooked meats, unpasteurized dairy products, and raw seafood.
Dietary Considerations for Individuals with Other Health Issues
Co-existing health conditions often influence dietary choices for ulcer management. The following considerations are essential for individuals managing multiple health concerns.
- Diabetes: The ulcer diet typically aligns well with a diabetes-friendly diet, focusing on whole grains, lean proteins, and avoiding sugary foods. Monitoring blood sugar levels is crucial. Choose low-glycemic index foods to help control blood sugar.
- Celiac Disease: Individuals with celiac disease must strictly avoid gluten. Many ulcer-friendly foods are naturally gluten-free, but carefully check food labels to avoid cross-contamination. Focus on fruits, vegetables, lean proteins, and gluten-free grains like rice and quinoa.
- Irritable Bowel Syndrome (IBS): The low-FODMAP diet, often used to manage IBS, can be adapted for ulcer management. This involves avoiding foods high in fermentable carbohydrates. Work with a registered dietitian to create a personalized meal plan.
- Kidney Disease: Individuals with kidney disease may need to limit protein and phosphorus intake. Coordinate your ulcer diet with your nephrologist to ensure your diet supports both ulcer healing and kidney health.
- High Blood Pressure: The ulcer diet, with its emphasis on low-sodium and unprocessed foods, is generally beneficial for managing high blood pressure. Limit salt intake and focus on fresh, whole foods.
Dietary Considerations for Individuals with Specific Medications
Certain medications can impact ulcer management and necessitate specific dietary adjustments.
- Blood Thinners: Medications like warfarin require careful monitoring of Vitamin K intake, as it can affect blood clotting. Maintain a consistent intake of Vitamin K-rich foods like leafy green vegetables to avoid fluctuations in medication effectiveness. Consult with your doctor or a registered dietitian to determine the appropriate amount for your situation.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs can increase the risk of ulcers. Taking these medications with food, especially ulcer-friendly foods, can help minimize stomach irritation. Avoid taking NSAIDs on an empty stomach.
- Antibiotics: Antibiotics can disrupt the gut microbiome, potentially leading to digestive issues. Consuming probiotic-rich foods like yogurt (if tolerated) or taking probiotic supplements may help restore gut health.
- Steroids: Long-term steroid use can increase the risk of ulcers. Following an ulcer-friendly diet can help mitigate this risk. Monitor for any new or worsening symptoms, and report them to your doctor.
Closing Notes
So there you have it, folks! The ulcer diet food list pdf isn’t just a list; it’s a lifestyle. It’s about taking control, making informed choices, and, most importantly, treating your tummy with the respect it deserves (even if it’s been a bit of a drama queen lately). Armed with this knowledge, you’re ready to face those ulcers head-on, armed with a fork and a whole lot of delicious, stomach-friendly foods.
Remember, a happy gut equals a happy you. Now go forth and conquer those ulcers, one delicious bite at a time!


