Whispers of a hidden malady, a fiery torment that flares in the joints, have led you here: printable gout food list pdf. The shadows of gout, cast by the accumulation of uric acid, beckon you into a world where every morsel holds a secret. You are about to delve into the cryptic realm of dietary choices, where the forbidden fruits and shrouded meats hold the key to easing the burden.
Gout, the ailment of kings and now, perhaps, you, arises from a shadowy imbalance within the body. It is a silent foe, a phantom menace, that is stirred by purines, those enigmatic compounds found in food. But fear not, for the path to redemption is laid bare in this guide, a printable gout food list pdf, a parchment of secrets, revealing the foods that dance on the edge of the abyss and those that offer solace.
Introduction: Understanding Gout and Dietary Management
Gout, a fiery whisper of inflammation, dances within the joints, a painful echo of the body’s own missteps. It arises from the silent accumulation of uric acid crystals, a consequence of the body’s struggle to process purines, the building blocks of life found in various foods. Managing this condition requires a multifaceted approach, and diet holds a pivotal role, acting as a shield against future flare-ups and a balm to soothe the present pain.
Defining Gout and Its Origins
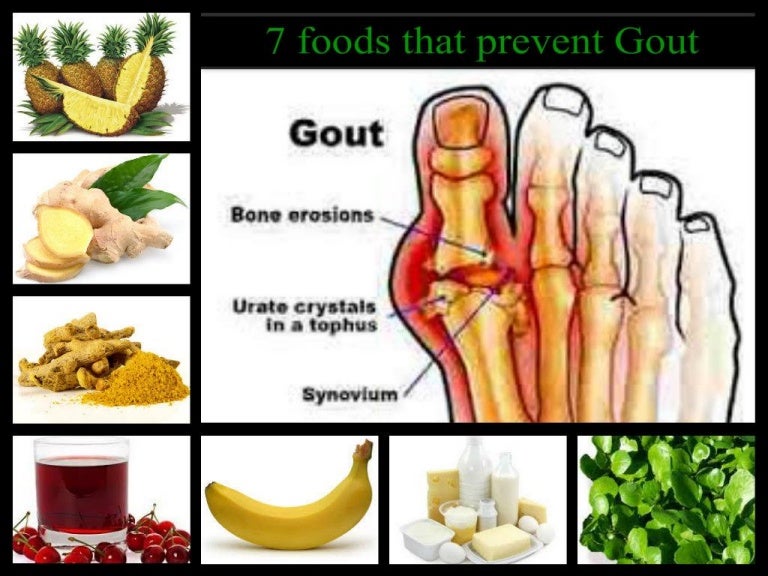
Gout is a form of inflammatory arthritis characterized by sudden, severe attacks of pain, swelling, redness, and tenderness in one or more joints, most commonly the big toe. This excruciating experience stems from hyperuricemia, a condition marked by elevated levels of uric acid in the blood. Uric acid is a byproduct of purine metabolism, and when the body produces too much uric acid or fails to eliminate it effectively, crystals of monosodium urate form and deposit in the joints, triggering an inflammatory response.
Diet’s Role in Gout Symptom Management
Dietary choices wield considerable influence over the management of gout. By carefully selecting foods, individuals can reduce the intake of purines, thereby lowering uric acid levels. Furthermore, certain foods possess anti-inflammatory properties that can help alleviate pain and swelling during a gout attack. The overarching goal of dietary management is to minimize the frequency and severity of gout flares, thereby improving the overall quality of life for those affected.
Importance of a Food List for Gout Sufferers
A meticulously crafted food list serves as an invaluable compass for individuals navigating the dietary landscape of gout. It provides a clear and concise guide, empowering individuals to make informed choices about the foods they consume. Such a list, ideally categorized into foods to avoid, foods to consume in moderation, and foods to embrace, facilitates the adoption of a gout-friendly diet.
By adhering to this guidance, individuals can significantly reduce their risk of flare-ups and maintain better control over their condition.
High-Purine Foods to Avoid
The path to managing gout requires a mindful approach to diet, specifically the avoidance of foods rich in purines. These compounds, when broken down by the body, produce uric acid, the culprit behind painful gout attacks. Understanding which foods to limit or eliminate is crucial for controlling uric acid levels and preventing flare-ups. This section provides a detailed guide to high-purine foods, categorized for clarity and ease of understanding.
Meats and Poultry
The realm of meats harbors some of the highest purine concentrations. Careful consideration is needed when incorporating these foods into your diet.
- Red Meats: Beef, lamb, and pork, particularly organ meats, are significant contributors to purine intake.
- Examples: Beefsteak, pork chops, lamb shanks.
- Safe Portion Size: Consider limiting red meat consumption to a maximum of 3-4 ounces per serving, and only a few times per month.
- Organ Meats: These include liver, kidneys, sweetbreads, and brains, and are exceptionally high in purines.
- Examples: Liver pâté, kidney stew, sweetbreads.
- Safe Portion Size: Avoid organ meats entirely. They are best excluded from the gout diet.
- Poultry: While generally lower in purines than red meat, certain preparations and cuts can still contribute significantly.
- Examples: Chicken, duck, turkey.
- Safe Portion Size: Skinless poultry, in moderation (3-4 ounces per serving), is generally acceptable. Avoid gravy made from poultry.
Seafood
The bounty of the sea, while nutritious, presents challenges for gout sufferers. Many seafood varieties are packed with purines.
- High-Purine Seafood: Certain types of seafood are best avoided due to their elevated purine content.
- Examples: Anchovies, sardines, herring, mackerel, scallops, mussels, and codfish.
- Safe Portion Size: Eliminate or severely limit consumption. If consumed, limit to very small portions (1-2 ounces) occasionally.
- Moderate-Purine Seafood: Some seafood options are lower in purines and can be included in moderation.
- Examples: Salmon, shrimp, lobster, crab, tuna.
- Safe Portion Size: Limit to 4-6 ounces per serving, a few times per week.
- Fish Roe: The eggs of fish are highly concentrated in purines.
- Examples: Caviar, fish roe used in sushi.
- Safe Portion Size: Avoid consumption entirely.
Other Foods
Beyond meats and seafood, other food items can contribute to elevated purine levels.
- Alcohol: Particularly beer and spirits, can trigger gout attacks.
- Examples: Beer, whiskey, vodka.
- Safe Portion Size: Eliminate beer entirely. Limit other alcoholic beverages to one drink per day, and consult a doctor.
- Sugary Drinks: Beverages high in fructose can increase uric acid levels.
- Examples: Soda, fruit juices with added sugar.
- Safe Portion Size: Avoid these beverages. Choose water or unsweetened alternatives.
- Certain Vegetables: While most vegetables are safe, a few contain moderate amounts of purines.
- Examples: Asparagus, spinach, mushrooms, cauliflower.
- Safe Portion Size: Consume in moderation (1/2 cup per serving). Generally, vegetables are beneficial for gout management.
Remember that individual tolerance varies. Always consult your healthcare provider or a registered dietitian to personalize your dietary plan and effectively manage your gout.
Moderate-Purine Foods
The path to managing gout, like a winding river, requires careful navigation. While high-purine foods represent treacherous rapids, moderate-purine foods present calmer waters, demanding mindful steering. These foods, though not forbidden, necessitate a considered approach to ensure the flow of well-being remains steady.
Identifying Moderate-Purine Foods
A careful selection is crucial in gout management. Certain foods, while not as laden with purines as the high-risk offenders, still contain a moderate amount that requires awareness.
- Meats: Moderate amounts of certain meats, particularly poultry (chicken, turkey) and some cuts of red meat, fall into this category. A small portion is generally considered acceptable.
- Seafood: Some seafood items, such as certain types of fish, like salmon and cod, and shellfish, including lobster and crab, are moderate in purine content.
- Vegetables: Some vegetables, such as asparagus, spinach, and mushrooms, contain moderate levels of purines. However, their overall nutritional benefits often outweigh the risks when consumed in moderation.
- Other Foods: Other items, such as certain types of beans and lentils, also contain moderate levels of purines.
Frequency and Portion Sizes for Moderate-Purine Food Consumption
The rhythm of consumption must be balanced to prevent a flare-up. The frequency and size of portions play a vital role in maintaining equilibrium.
The recommended approach often involves consuming moderate-purine foods in controlled portions and with careful attention to overall dietary balance. A typical guideline might suggest limiting servings to a few times per week, adjusting based on individual tolerance and the severity of gout symptoms. For example, a small serving of salmon (around 3-4 ounces) once or twice a week could be acceptable, while larger or more frequent portions might increase the risk of a gout attack.
“Moderation is key. Small portions, infrequent consumption, and mindful choices are your allies in this journey.”
Impact of Cooking Methods on Purine Content
The alchemical transformation of cooking can subtly alter the purine content of food. Certain methods may influence the concentration of purines, necessitating an understanding of how to cook wisely.
The cooking method can affect the purine levels in food. For instance, boiling meat and discarding the cooking water can reduce the purine content, as purines are water-soluble and leach out during the cooking process. Conversely, methods like frying or grilling, which do not involve discarding cooking liquids, may retain more purines.
Consider the example of cooking chicken. Boiling chicken and discarding the broth can remove a significant portion of purines. However, if the chicken is grilled and the drippings are consumed, the purine content remains relatively unchanged. The choice of cooking method, therefore, is another tool in the gout sufferer’s arsenal, allowing for more informed choices about food preparation.
Low-Purine Foods: The Cornerstone of a Gout-Friendly Diet
The path to managing gout often winds through the kitchen, where mindful food choices can become powerful allies. Embracing a diet rich in low-purine foods is akin to laying the foundation for a stable and healthy life, minimizing the risk of painful flare-ups. This section illuminates the bounty of foods that can be savored without undue worry, empowering you to create delicious and gout-friendly meals.
Low-Purine Food Groups and Examples
A diet designed to minimize purine intake necessitates a focus on specific food groups, each offering a unique contribution to well-being. The following list details key groups and the nourishing examples they contain, offering a guide to building a vibrant and gout-conscious menu.
- Fruits: Nature’s candy, fruits are generally low in purines and provide essential vitamins and antioxidants.
- Apples: Crisp and refreshing, apples offer a satisfying crunch and are packed with fiber.
- Berries (strawberries, blueberries, raspberries): These vibrant jewels burst with flavor and are rich in antioxidants, fighting inflammation. Imagine a bowl overflowing with these colorful delights.
- Cherries: Known for their potential anti-inflammatory properties, cherries can be a delicious addition. Consider a handful of fresh cherries or a glass of tart cherry juice.
- Citrus fruits (oranges, grapefruit): These zesty fruits are a source of vitamin C, which may help reduce uric acid levels.
- Pears: A sweet and juicy option, pears are a good source of fiber.
- Vegetables: The cornerstone of a healthy diet, most vegetables are low in purines.
- Leafy Greens (spinach, kale, lettuce): These nutrient-packed greens are versatile and can be enjoyed in salads, smoothies, or cooked dishes. Visualize a vibrant salad overflowing with various greens.
- Broccoli: This cruciferous vegetable offers a wealth of vitamins and minerals.
- Carrots: Sweet and crunchy, carrots are a good source of beta-carotene.
- Cucumbers: Refreshing and hydrating, cucumbers are a great addition to salads and sandwiches.
- Peppers (bell peppers): Available in various colors, bell peppers add flavor and nutrients to any meal.
- Tomatoes: Though sometimes debated, tomatoes are generally considered safe in moderation.
- Grains: Opt for whole grains for sustained energy and fiber.
- Whole wheat bread: Choose whole-grain varieties over refined white bread.
- Oats: A warm and comforting breakfast option, oats are a good source of soluble fiber.
- Rice (white and brown): White rice is generally lower in purines than brown rice, but brown rice offers more fiber.
- Pasta: Choose whole-wheat pasta for added fiber.
- Dairy Products: Dairy, especially low-fat options, can be beneficial.
- Low-fat milk: A good source of calcium and protein.
- Yogurt (low-fat): Provides probiotics for gut health.
- Cheese (in moderation, especially low-fat varieties): A source of calcium and protein.
- Beverages: Choose wisely to support hydration and health.
- Water: The most important beverage for hydration and overall health.
- Coffee (in moderation): Studies suggest coffee may have a protective effect.
- Tea (herbal and green): Offers antioxidants and hydration.
- Low-purine fruit juices: Choose options without added sugars.
- Fats: Healthy fats can contribute to a balanced diet.
- Olive oil: A staple of the Mediterranean diet, known for its heart-healthy benefits.
- Avocado: Provides healthy fats and fiber.
Sample Meal Plan Incorporating Low-Purine Foods
Crafting a gout-friendly meal plan doesn’t mean sacrificing flavor or variety. The following sample plan demonstrates how to incorporate low-purine foods throughout the day, creating a balanced and satisfying eating experience. This is a model, and individual needs may vary.
| Meal | Food Examples |
|---|---|
| Breakfast | Oatmeal with berries and low-fat milk, a side of orange slices, and a cup of green tea. |
| Lunch | Large salad with mixed greens, cucumber, bell peppers, carrots, grilled chicken (in moderation), and a light olive oil and vinegar dressing. A slice of whole-wheat bread. |
| Dinner | Baked salmon (in moderation) with steamed broccoli, quinoa, and a side of fresh fruit. |
| Snacks (optional) | A handful of berries, a small serving of yogurt, or a few carrot sticks with hummus. |
| Beverages Throughout the Day | Water, herbal tea, and coffee (in moderation). |
This meal plan emphasizes a balance of fruits, vegetables, whole grains, and lean protein (in moderation). Portion sizes should be adjusted to meet individual caloric needs and activity levels. Consulting with a healthcare professional or a registered dietitian is always recommended to personalize a diet plan that best suits your individual health requirements and preferences.
Beverages and Gout: Printable Gout Food List Pdf
The choice of beverages plays a significant role in managing gout, as some drinks can trigger flare-ups, while others can offer protection. Hydration and the types of liquids consumed are crucial aspects of dietary management for individuals with gout. This section explores the impact of various beverages, providing insights into what to embrace and what to avoid for optimal health.
Impact of Beverages on Gout, Printable gout food list pdf
The beverages consumed can significantly influence uric acid levels in the body, a key factor in gout. Certain drinks contribute to the buildup of uric acid, leading to painful joint inflammation, while others aid in its excretion, potentially reducing the frequency and severity of gout attacks. Understanding these effects is paramount in creating a gout-friendly diet.
Comparing Water, Coffee, Tea, and Sugary Drinks
Different beverages have varying effects on uric acid levels and overall gout management. The choice of drink can impact the body’s ability to process purines and eliminate uric acid.
- Water: Water is the cornerstone of gout management. Adequate hydration helps the kidneys flush out uric acid, reducing the risk of crystal formation in the joints. It is essential to drink plenty of water throughout the day. Consider carrying a reusable water bottle and refilling it frequently as a visual reminder.
- Coffee: Studies suggest that coffee consumption may be associated with a lower risk of gout. Coffee can inhibit the enzyme xanthine oxidase, which is involved in uric acid production. However, the exact mechanism is still being researched, and individual responses may vary. One study, published in the
-Annals of the Rheumatic Diseases*, followed over 45,000 men for 12 years and found that those who consumed more coffee had a lower risk of developing gout. - Tea: The effects of tea on gout are less clear than those of coffee. Some studies indicate that tea, particularly green tea, may have anti-inflammatory properties that could benefit gout sufferers. However, the purine content in tea varies, and excessive consumption might not be beneficial. More research is needed to establish a definitive link between tea consumption and gout.
- Sugary Drinks: Sugary drinks, including sodas and fruit juices, are strongly linked to an increased risk of gout. These beverages are high in fructose, which can increase uric acid production. The consumption of fructose-sweetened beverages has been consistently associated with higher uric acid levels and a greater likelihood of gout attacks. The American College of Rheumatology recommends limiting or avoiding these drinks to manage gout effectively.
For example, in a study published in the
-British Medical Journal*, researchers found that drinking one or two servings of sugary drinks per day increased the risk of gout by 85%.
Beverages to Avoid and Beverages that Can Be Beneficial
Making informed choices about beverages is a critical aspect of gout management. Identifying drinks to avoid and those that can be beneficial can significantly impact the frequency and severity of gout attacks.
- Beverages to Avoid: High-fructose corn syrup sweetened beverages, such as sodas and fruit juices, should be avoided. Alcoholic beverages, particularly beer (due to its high purine content and alcohol’s impact on uric acid metabolism) and spirits, should also be limited or avoided.
- Beverages that Can Be Beneficial: Water is the primary beverage of choice, and drinking plenty of it helps to flush out uric acid. Coffee, in moderation, may offer benefits. Tea, especially green tea, may have anti-inflammatory properties. Consider these choices as part of a well-balanced gout-friendly diet.
Sample Meal Plans
To navigate the culinary landscape of gout, one needs a compass of flavorful, low-purine dishes. The following meal plans offer a glimpse into a gout-friendly diet, providing a foundation for creating delicious and health-conscious meals. These plans are designed to be a starting point, allowing for personalization based on individual preferences and dietary needs. Remember to consult with a healthcare professional or a registered dietitian for personalized advice.
3-Day Sample Meal Plan with Recipes
The following meal plan Artikels three days of meals, each meticulously crafted to prioritize low-purine ingredients. Each meal suggestion includes a brief recipe description and an estimated nutritional breakdown, including calories and purine content. Please note that purine content is approximate and can vary based on specific ingredients and preparation methods. The focus remains on foods that are generally considered low in purines, supporting a healthy and gout-conscious lifestyle.
| Day | Meal | Recipe/Meal Description | Approximate Calories | Approximate Purine Content (mg) |
|---|---|---|---|---|
| Day 1 | Breakfast | Oatmeal with Berries and Almonds: Prepare a serving of oatmeal with water or low-fat milk. Top with a handful of fresh berries (strawberries, blueberries) and a sprinkle of almonds. | 350 | 10 |
| Lunch | Chicken Salad Sandwich on Whole-Wheat Bread: Use cooked chicken breast (low-purine). Combine with mayonnaise, celery, and a touch of Dijon mustard. Serve on whole-wheat bread with a side of mixed greens. | 450 | 50 | |
| Dinner | Baked Salmon with Roasted Vegetables: Bake a salmon fillet (a moderate-purine food, portion control is key). Roast a mix of low-purine vegetables like bell peppers, zucchini, and onions with olive oil and herbs. | 550 | 75 | |
| Day 2 | Breakfast | Scrambled Eggs with Spinach and Toast: Scramble two eggs with a handful of fresh spinach. Serve with a slice of whole-wheat toast. | 300 | 20 |
| Lunch | Lentil Soup with a Side Salad: Prepare a hearty lentil soup (lentils are moderate-purine, consume in moderation). Serve with a side salad of mixed greens, cucumbers, and tomatoes with a light vinaigrette. | 400 | 70 | |
| Dinner | Chicken Stir-Fry with Rice: Stir-fry chicken breast with a variety of low-purine vegetables such as broccoli, carrots, and snow peas. Serve over a bed of white rice. | 600 | 60 | |
| Day 3 | Breakfast | Greek Yogurt with Fruit and Granola: Enjoy a serving of plain Greek yogurt. Top with your choice of fresh fruit (bananas, peaches) and a small amount of granola. | 380 | 15 |
| Lunch | Turkey Breast and Vegetable Wrap: Use a whole-wheat tortilla to create a wrap filled with sliced turkey breast (low-purine), lettuce, tomato, and a light dressing. | 420 | 45 | |
| Dinner | Pasta with Tomato Sauce and Vegetables: Prepare pasta (choose whole-wheat) and top with a homemade tomato sauce rich in vegetables like carrots, zucchini, and bell peppers. | 500 | 30 |
It’s important to remember that individual purine tolerance varies. The key is to observe how different foods affect your symptoms and adjust your diet accordingly, always under the guidance of a healthcare professional.
Cooking Methods and Preparation Techniques
The art of preparing gout-friendly meals extends beyond ingredient selection. It encompasses the techniques employed in the kitchen, where seemingly small choices can significantly impact purine levels in your food. Understanding and utilizing specific cooking methods can be a powerful tool in managing gout symptoms and promoting overall well-being. The goal is to minimize purine intake while maximizing flavor and nutritional value.
Cooking Methods to Reduce Purine Content
Certain cooking techniques can help leach purines from food, making them more suitable for those managing gout. These methods often involve the use of water or other liquids to draw out purines.Boiling is a method that can reduce purine content. By boiling ingredients in water, some purines are dissolved and transferred into the cooking liquid. This is particularly effective for foods like meat and poultry.Grilling, with its high-heat, dry-cooking approach, doesn’t remove purines.
It can even concentrate them if the food is cooked for an extended period, as some moisture evaporates, and the purines remain.Steaming is gentler than boiling, and while it may not reduce purine content as effectively, it preserves more nutrients and flavors. Steaming can be a healthy alternative to grilling, especially for vegetables.
Comparing Boiling, Grilling, and Steaming
Each cooking method presents unique advantages and disadvantages when it comes to managing purine intake. The choice of method should consider both purine reduction and the desired taste and texture of the meal.Boiling, as mentioned, is the most effective at reducing purine levels. However, it can also lead to a loss of some water-soluble vitamins and alter the texture of the food.
The cooking liquid, now rich in purines, should be discarded. For example, when preparing a broth, using the boiled meat for the broth is not recommended.Grilling, on the other hand, doesn’t remove purines. In fact, it can potentially concentrate them. It is best to avoid grilling high-purine foods. However, grilling can be a suitable method for low-purine foods, such as certain vegetables.Steaming is a middle ground.
It retains more nutrients than boiling and doesn’t concentrate purines like grilling. While it doesn’t reduce purine levels significantly, it’s a healthier choice than grilling, especially for vegetables.
Tips for Preparing Gout-Friendly Meals
Implementing these techniques can help create delicious and gout-conscious meals.* Choose Low-Purine Ingredients: Start with a foundation of low-purine foods, such as fruits, vegetables, and whole grains.
Trim Excess Fat
Remove visible fat from meats before cooking. Fat can contribute to inflammation, which may worsen gout symptoms.
Use Boiling Wisely
When boiling meat or poultry, discard the cooking liquid. This will help remove purines.
Embrace Steaming
Steam vegetables to retain nutrients and avoid adding extra fats.
Season with Herbs and Spices
Enhance flavor with herbs and spices instead of relying on salt or high-sodium seasonings.
Plan Your Meals
Meal planning helps ensure you have the right ingredients on hand and can avoid impulsive high-purine food choices.
Read Labels
Pay attention to food labels and ingredient lists, particularly for hidden sources of purines or high-fructose corn syrup.
Hydrate
Drink plenty of water throughout the day to help flush out excess uric acid.
The Importance of Hydration
Within the intricate dance of gout management, hydration emerges not merely as a supporting player, but as a principal partner. Water, the elixir of life, plays a crucial role in mitigating the painful flares that characterize this inflammatory arthritis. Its influence extends beyond mere quenching of thirst, touching upon the very mechanisms that govern uric acid levels and the health of the kidneys.
Daily Water Intake Guidelines
The body’s need for water is a constant, yet the specific requirements can fluctuate based on individual factors. General recommendations offer a starting point, but personalization is key.
The general recommendation for daily water intake is around 8 glasses of water (approximately 2 liters or 64 ounces).
This is a baseline, and adjustments are often necessary.* Individual Factors: Consider factors such as activity level, climate, and overall health. Those who are more active, live in warmer climates, or have certain medical conditions may require more water.
Monitoring Urine Color
A simple method for assessing hydration status involves observing urine color. Pale yellow urine generally indicates adequate hydration, while darker urine suggests the need for increased fluid intake.
Listen to Your Body
Thirst is a fundamental signal. Responding promptly to thirst cues is essential. However, waiting until thirst strikes can mean the body is already experiencing some degree of dehydration.
Benefits of Staying Hydrated
Adequate hydration offers a multitude of benefits in the context of gout, impacting both the immediate symptoms and the long-term management of the condition.* Uric Acid Dilution: Water helps dilute uric acid in the bloodstream, reducing the likelihood of crystal formation. This dilution makes it less likely for the uric acid to precipitate out and form crystals in the joints.
Enhanced Kidney Function
The kidneys are the primary organs responsible for filtering uric acid from the blood. Hydration supports optimal kidney function, facilitating efficient uric acid excretion.
Prevention of Kidney Stones
High uric acid levels can contribute to the formation of kidney stones, a painful complication of gout. Adequate fluid intake helps to prevent stone formation by flushing out uric acid.
Reduced Flare Frequency and Severity
Proper hydration can lessen the frequency and intensity of gout flares. By keeping uric acid levels in check, hydration helps to minimize the inflammatory response.
Improved Joint Health
Hydration contributes to overall joint health. Water acts as a lubricant for the joints, helping to reduce friction and pain.
Example
Case Study – Mr. Evans: Mr. Evans, a 62-year-old diagnosed with gout, was experiencing frequent and debilitating flares. After implementing a daily regimen of increased water intake, along with dietary adjustments, he noted a significant decrease in the frequency and severity of his gout attacks. He also reported a reduction in joint stiffness and improved overall mobility.
This illustrates the tangible benefits of consistent hydration in managing gout.
Supplements and Gout
The realm of supplements offers a glimmer of hope for managing gout symptoms, yet it’s a landscape fraught with complexities. While some supplements may offer relief, others can exacerbate the condition or interact negatively with medications. Navigating this terrain requires careful consideration and consultation with a healthcare professional. This section delves into the potential benefits and risks of specific supplements, highlighting those that may prove beneficial and cautioning against potential pitfalls.
Potential Benefits and Risks of Supplements
The allure of supplements lies in their promise of providing essential nutrients or compounds that may support overall health and, in the context of gout, help manage inflammation and uric acid levels. However, the regulatory landscape for supplements is less stringent than for pharmaceuticals, meaning that their efficacy and safety can vary significantly. Understanding the potential benefits and risks is paramount before incorporating any supplement into a gout management plan.* Benefits: Some supplements, like vitamin C and cherry extract, have shown promise in reducing uric acid levels and mitigating inflammation.
Others, such as omega-3 fatty acids, may support overall health and reduce the risk of cardiovascular complications often associated with gout.
Risks
The risks associated with supplements range from mild side effects to serious interactions with medications. Some supplements may interfere with the effectiveness of gout medications, while others could worsen kidney function, a concern for individuals with gout. The quality and purity of supplements can also vary, leading to inconsistencies in their effects.
Supplements that May Help Manage Gout Symptoms
Several supplements have demonstrated potential benefits in managing gout symptoms, although more research is often needed to confirm these findings. These supplements typically work by reducing uric acid levels, decreasing inflammation, or providing essential nutrients. It is crucial to consult with a healthcare provider before using any of these supplements, as they may not be suitable for everyone.* Vitamin C: Vitamin C acts as an antioxidant and has been shown in some studies to reduce uric acid levels in the blood.
The recommended daily intake for gout management varies, but dosages up to 500mg per day have been used in clinical trials.
Cherry Extract
Both cherry extract and cherry juice have been traditionally used and studied for their potential to reduce gout flares. They contain anthocyanins, which have anti-inflammatory properties. Research suggests that consuming cherries or cherry extract may lower uric acid levels and reduce the frequency of gout attacks.
Omega-3 Fatty Acids
Found in fish oil, omega-3 fatty acids have anti-inflammatory effects that may help reduce joint pain and inflammation associated with gout. While not directly impacting uric acid levels, they contribute to overall health and may reduce the risk of cardiovascular complications.
Bromelain
This enzyme, found in pineapple, has anti-inflammatory properties and may help reduce pain and swelling. It’s often used as a complementary therapy for joint pain, including that associated with gout.
Turmeric (Curcumin)
Curcumin, the active compound in turmeric, is a potent anti-inflammatory agent. Some studies suggest that curcumin may help reduce pain and inflammation in gout. However, the bioavailability of curcumin is often low, so formulations with enhanced absorption may be preferred.
Warnings Regarding Supplements and Potential Interactions
The use of supplements, while potentially beneficial, is not without risk. It’s essential to be aware of potential interactions with medications and to consider the individual’s overall health profile. Consulting with a healthcare professional is critical to ensure the safe and effective use of supplements.* Medication Interactions: Some supplements can interact with gout medications, such as allopurinol and colchicine, altering their effectiveness or increasing the risk of side effects.
For example, vitamin C, in high doses, might interfere with the efficacy of certain medications.
Kidney Function
Individuals with gout often have impaired kidney function. Certain supplements, such as high doses of vitamin C or creatine, could potentially strain the kidneys, exacerbating existing problems.
Individual Sensitivities
People can have individual sensitivities or allergies to ingredients in supplements. It’s important to read labels carefully and be aware of potential allergens.
Quality and Purity
Obtain direct knowledge about the efficiency of vietnamese food gluten free through case studies.
The supplement industry is not as strictly regulated as the pharmaceutical industry. The quality and purity of supplements can vary, so choosing reputable brands and looking for third-party certifications (such as USP, NSF International, or ConsumerLab.com) is advisable.
Dosage and Timing
Adhering to recommended dosages and timing is critical. Taking excessive amounts of certain supplements can be harmful. Following the advice of a healthcare provider is essential.
Example of Interaction
Consider a patient taking allopurinol to reduce uric acid levels. If this patient starts taking high doses of vitamin C without consulting a doctor, it could potentially reduce the effectiveness of the allopurinol, leading to elevated uric acid levels and gout flares.
Creating a Printable Food List
The creation of a user-friendly, printable food list is paramount in empowering individuals managing gout through dietary adjustments. This tangible resource serves as a readily accessible guide, enabling informed food choices and facilitating adherence to a gout-friendly diet. Its design should prioritize clarity, conciseness, and ease of use, allowing for quick reference and consistent application in daily meal planning.
Structure and Format
The printable food list will be structured using an HTML table, designed for readability and responsiveness across various devices. This table will employ four distinct columns to provide comprehensive information on each food item. The layout ensures information is presented in an organized and easily digestible manner, aiding in effective dietary management.
| Food | Purine Level | Notes | Serving Size & Recommendations |
|---|---|---|---|
| Anchovies | Very High | Avoid entirely | 0 g (Avoid) |
| Spinach | Moderate | Consume in moderation | 1 cup cooked (Limit to 1-2 servings per week) |
| Cherries | Low | May help reduce gout flares | 1 cup (Enjoy daily) |
| Water | N/A | Essential for hydration | 8 glasses per day (Minimum) |
Each column serves a specific purpose in providing relevant information:
- Food: This column lists the name of the food item. Examples include “Anchovies,” “Spinach,” “Cherries,” and “Water.” The food names are clearly stated to avoid confusion.
- Purine Level: This column categorizes each food item based on its purine content. Categories include “Very High,” “High,” “Moderate,” and “Low,” providing a quick reference for dietary choices.
- Notes: This column offers additional information about the food item, such as specific recommendations, potential benefits, or any relevant warnings. For example, it might state, “May help reduce gout flares” for cherries.
- Serving Size & Recommendations: This column specifies the recommended serving size and provides practical advice on how the food item can be incorporated into a gout-friendly diet. This may range from “Avoid entirely” for high-purine foods to “Enjoy daily” for beneficial items.
This format allows for easy scanning and understanding, making the food list a valuable tool for individuals managing gout. The clear presentation of information supports informed decision-making and facilitates consistent dietary adherence.
Lifestyle Factors and Gout: Beyond Diet
The path to managing gout extends far beyond the plate, encompassing a holistic approach to well-being. While diet is a crucial cornerstone, several lifestyle factors significantly influence the frequency and severity of gout flares. Understanding and addressing these elements can empower individuals to take control of their health and reduce the impact of this painful condition.
The Significance of Exercise and Weight Management
Physical activity and maintaining a healthy weight are paramount in mitigating gout symptoms. Excess weight, particularly around the abdomen, can lead to increased uric acid production and decreased uric acid excretion by the kidneys, thus creating a favorable environment for gout flares. Regular exercise helps in weight management, improving insulin sensitivity, and potentially reducing uric acid levels.
- Weight Management: Gradual and sustainable weight loss is recommended. Rapid weight loss can sometimes worsen gout flares due to the breakdown of cells, releasing purines. Aim for a healthy BMI (Body Mass Index) through a balanced diet and regular exercise.
- Aerobic Exercise: Activities like brisk walking, swimming, and cycling for at least 150 minutes per week, spread throughout the week, are beneficial. These exercises help burn calories, improve cardiovascular health, and potentially reduce uric acid levels.
- Strength Training: Incorporating strength training exercises, such as lifting weights or using resistance bands, twice a week can help build muscle mass, which in turn can boost metabolism and aid in weight management.
- Avoid Overexertion: While exercise is crucial, avoid overexertion, especially during a gout flare. Excessive physical stress can sometimes trigger a flare.
- Consult a Healthcare Professional: Before starting any new exercise program, consult with a doctor or physical therapist, especially if you have underlying health conditions. They can help create a safe and effective exercise plan tailored to your needs.
Stress Management Techniques
Stress, both physical and emotional, can be a significant trigger for gout flares. Stress hormones can impact uric acid levels and inflammation in the body. Employing effective stress management techniques is crucial for overall health and gout management.
- Mindfulness and Meditation: Practicing mindfulness and meditation can help reduce stress levels and promote a sense of calm. Regular meditation can help lower cortisol levels, a stress hormone, and improve overall well-being. Consider guided meditation apps or classes.
- Deep Breathing Exercises: Deep breathing exercises can quickly calm the nervous system and reduce stress. Practice taking slow, deep breaths, inhaling through your nose and exhaling through your mouth.
- Yoga and Tai Chi: These practices combine physical postures, breathing techniques, and meditation, offering a holistic approach to stress management. They can improve flexibility, reduce muscle tension, and promote relaxation.
- Adequate Sleep: Aim for 7-9 hours of quality sleep per night. Sleep deprivation can increase stress levels and worsen gout symptoms. Establish a regular sleep schedule and create a relaxing bedtime routine.
- Social Support: Connecting with friends, family, or support groups can provide emotional support and reduce feelings of isolation. Sharing your experiences and seeking advice from others can be beneficial.
- Hobbies and Relaxation: Engage in activities you enjoy, such as reading, listening to music, or spending time in nature. These activities can help you relax and de-stress.
- Professional Counseling: If stress is overwhelming, consider seeking professional help from a therapist or counselor. They can provide tools and strategies for managing stress effectively.
Frequently Asked Questions (FAQ)
The path to managing gout often winds through a maze of inquiries. This section seeks to illuminate the most common queries, dispelling myths and offering clarity on the crucial interplay between diet and this inflammatory ailment. Understanding these answers empowers individuals to navigate their dietary choices with confidence, fostering a proactive approach to their well-being.
Common Misconceptions About Gout and Diet
Many misunderstandings cloud the understanding of gout and its dietary management. Recognizing these flawed beliefs is the first step toward adopting effective strategies.
- The belief that gout is solely caused by eating high-purine foods. While purines play a role, factors like genetics, kidney function, and overall lifestyle significantly contribute to the disease’s development.
- The assumption that avoiding all purines is necessary. A complete avoidance of purines is impractical and potentially detrimental to overall health. The focus should be on managing intake rather than complete elimination.
- The misconception that all alcoholic beverages have the same effect. While beer and spirits are often higher in purines, the impact of wine can vary, often with lower purine content. Moderation and individual tolerance are key.
- The idea that diet alone can cure gout. Dietary adjustments are crucial, but they are often most effective when combined with medication and other lifestyle modifications, as prescribed by a healthcare professional.
- The false notion that gout only affects older men. Gout can affect anyone, including women and younger individuals, although it is more prevalent in certain demographics.
Frequently Asked Questions and Concise Answers
Navigating the complexities of gout necessitates clear, concise answers to common queries. This section provides direct responses to facilitate understanding and informed decision-making.
- What is gout? Gout is a form of arthritis characterized by sudden, severe attacks of pain, swelling, redness, and tenderness in one or more joints, most often the big toe. It’s caused by a buildup of uric acid crystals in the joints.
- How does diet affect gout? Dietary choices significantly impact gout. High-purine foods can increase uric acid levels, triggering gout attacks. A diet focused on low-purine foods can help manage these levels and reduce the frequency of attacks.
- Which foods should be avoided to manage gout? Foods high in purines, such as red meat, organ meats (liver, kidney, etc.), certain seafood (anchovies, sardines, etc.), and beer, should be limited or avoided.
- What foods are considered gout-friendly? A gout-friendly diet emphasizes low-purine foods like fruits, vegetables, whole grains, and low-fat dairy products. Water is also crucial for flushing out uric acid.
- Can I drink alcohol if I have gout? Moderate alcohol consumption may be acceptable, but beer and spirits are generally discouraged due to their high purine content. Wine may be consumed in moderation, but it’s important to monitor its effects.
- Does drinking coffee or tea affect gout? Research suggests that moderate coffee consumption may be associated with a lower risk of gout. Tea’s impact is less clearly defined, but generally considered safe in moderation.
- What is the role of hydration in managing gout? Adequate hydration is essential. Drinking plenty of water helps the kidneys flush out uric acid, reducing the risk of crystal formation and gout attacks.
- Can supplements help manage gout? Some supplements, like vitamin C and cherries, may offer some benefits, but they should be discussed with a healthcare provider. They should not replace prescribed medication.
- How can I create a gout-friendly meal plan? Focus on low-purine foods, moderate portion sizes, and balanced meals. Consult with a registered dietitian or healthcare provider for personalized guidance.
- Is it possible to completely eliminate gout attacks through diet alone? While diet plays a significant role, it may not completely eliminate attacks. It often works best in conjunction with medication and other lifestyle changes, like maintaining a healthy weight.
- How does weight management affect gout? Maintaining a healthy weight is crucial. Obesity increases uric acid levels and the risk of gout attacks. Weight loss can help reduce these levels and improve gout management.
- Should I avoid all animal products? Not necessarily. While red meat and organ meats should be limited, moderate consumption of other animal products, like lean poultry and fish (in moderation), may be included in a balanced diet.
Ending Remarks
As you emerge from this culinary quest, armed with your printable gout food list pdf, you will find the shadowy world of gout now illuminated. You have learned the dance of purines, the secrets of hydration, and the power of mindful eating. Remember that this journey is not merely about what you avoid, but what you embrace: a symphony of flavors, a tapestry of health, and the quiet triumph over a hidden enemy.
May your joints find peace, and your path be clear.


